Your Sluice Sink Passed Inspection—But Is It Clinically Effective
In the highly regulated world of healthcare facility design and hospital equipment procurement, achieving regulatory compliance is often, and understandably, viewed as the final measure of success. Certification is acquired, the equipment is installed, and the immediate risk of sanctions is mitigated. Yet, particularly in high-traffic, high-biohazard areas like the dirty utility room, this reliance on minimum standards often creates a significant and continuous clinical risk. For architects, facility managers, and procurement officers, the pivotal question must shift: “Is our compliant sluice sink truly effective in the relentless, real-world battle against Healthcare-Associated Infections (HAIs)?”
Foundational industry standards, such as HTM 64 2, establish a crucial framework for hygiene, durability, and space planning. However, adherence to this regulatory baseline frequently results in the acquisition of what we term the “Minimum Viable Sluice” (MVS). The MVS satisfies the regulatory checklist but exhibits a significant functional gap when confronted with the actual, rigorous demands of modern clinical hygiene standards. This performance deficit translates directly into massive financial exposure. HAIs cost U.S. hospitals annually between $28.4 billion and $45 billion. This overwhelming data confirms that any initial Capital Expenditure (CAPEX) savings achieved by selecting a cheaper, compliant-only sluice sink are negligible compared to the expenses incurred by even a single outbreak.
Clinical Effectiveness: A Working Definition
In the context of this technical analysis, “Clinical Effectiveness” refers specifically to a piece of equipment’s sustained infection control performance and its clinical risk mitigation capacity within the high-stress, real-world operational environment of a hospital. It measures the product’s comprehensive ability to reduce pathogen persistence and minimize the opportunity for cross-contamination.
The fundamental objective must be to elevate the standard of success from mere inspection compliance to verifiable, sustained infection control performance. This paper is designed to reveal that, in the domain of infection control, merely satisfying minimum compliance is a high-risk strategic choice. True safety stems from the proactive pursuit of clinical effectiveness—a verifiable performance standard built on superior material science, precision engineering, and human factors design. But where exactly do minimum compliance standards fall short of this rigorous definition? The following analysis reveals the structural flaws in accepting the status quo.
I. Where Minimum Standards Fail
A. The Structural Flaw in Basic Compliance
Regulatory guidelines properly emphasize features that minimize infection transmission risk and demand the use of durable materials. However, the framework’s flexibility on material specifics—such as merely requiring “stainless steel” without a specific grade or mandated surface finish metrology—actively incentivizes the substitution of materials based on initial cost. This decision, while meeting the letter of the law 1, severely compromises the long-term clinical objective.
The environment within the dirty utility room subjects sluice washing sinks to constant exposure to highly aggressive cleaning chemicals, chlorides, and biological waste. A critical deficiency in many compliant-only sluice sinks is insufficient chemical resilience. Standard SS 304, often chosen for cost-effectiveness, lacks the inherent capacity to withstand the rigorous, high-intensity disinfection cycles required to combat contemporary drug-resistant organisms.
This material inadequacy causes microscopic surface degradation, primarily through pitting. Once this degradation occurs, the surface—though certified as “durable”—is functionally compromised, creating protected micro-habitats for persistent pathogens.
B. Material Failure as a Financial Liability
The financial consequence of accepting inadequate material standards is significant and measurable. This data necessitates a shift in strategic thinking from prioritizing low CAPEX (Capital Expenditure) to managing Total Cost of Ownership (TCO).
| Financial Impact Indicator | Minimum Compliance Standard: Cost Burden (e.g., SS 304) | Clinical Efficacy Standard: ROI & Cost Avoidance (e.g., SS 316) |
|---|---|---|
| Pitting/Corrosion Risk | High: Inevitable degradation from hypochlorite cleaners. | Low: SS 316 offers superior chemical resilience. |
| Pathogen Persistence Risk | High: Pits shelter biofilms, leading to chronic contamination. | Low: Surface integrity maintained, reducing biofilm establishment sites. |
| Total Cost of Ownership (TCO) | High: Increased maintenance, early replacement CAPEX, and significant HAI liability. | Low: Extended operational lifespan, minimal corrective maintenance, and effective cost avoidance. |
The acceptance of a material that is structurally unable to withstand the chemical intensity required for modern hygiene often leads to material failure, which brings with it a long-term hygiene compromise and elevated TCO. This underscores the need for facilities procurement to integrate risk management strategy directly into material specification.
C. Where Compliance Fails
Procurement officers and hospital maintenance teams frequently encounter compliant systems that introduce clinical risk:
- The Aerosolization Hazard: A sluice sink is installed with a standard deep basin and high-pressure faucet, meeting spatial requirements. However, studies confirm that the combination of sink basin depth and water flow rate can cause pathogens from the drain to spread to adjacent environmental surfaces through aerosolization. The required process of cleaning inadvertently transforms the utility sink into an active fomite, spreading pathogens across the dirty utility room and potentially into clean areas.
- The Biofilm Sanctuary: When a standard sink’s surface degrades, microscopic pitting provides a refuge for biofilm communities. Biofilms are communities of microorganisms encased in a protective layer, making them approximately 1,000 times harder to kill than free-floating microbes. The compliant sink, having passed inspection, becomes a guaranteed environmental contamination reservoir.
The transition to building a clinically effective sluice sink must, therefore, fundamentally address the material and design shortcomings at their source. This commitment is founded on three core pillars.
II. Engineering for Risk Mitigation
A clinical sluice sink must be engineered with integrated features to achieve passive pathogen denial (via material science) and active waste containment (via design geometry).
A. Pillar One: The Necessity of SS 316 and Surface Integrity
The choice of stainless steel grade determines the fixture’s long-term surface integrity against chemical stressors.
1. The Strong Case for SS 316
In environments requiring high-level clinical effectiveness, generic stainless steel is inadequate. The technical necessity for SS 316 lies in the addition of Molybdenum to the alloy. This element provides crucial resilience against chlorides and other aggressive chemical agents. This enhanced chemical resilience is the fundamental prerequisite for preventing the micro-pitting that otherwise accelerates material degradation. The strategic investment in SS 316 is a direct application of material science leveraged to secure long-term infection control performance. It provides a level of assurance that exceeds the base regulatory standard for high-stress applications.
2. Material Failure as a Microbiological Catalyst
For the facility manager, material corrosion must be viewed not as a structural failure but as a microbiological vulnerability. Each corrosive pit, often microscopically small, creates an ideal sanctuary for biofilm communities. These sheltered depressions protect establishing persistent pathogens from routine chemical disinfectants, thereby rendering the entire sluice sink system clinically compromised. The superior resilience of SS 316 translates directly into long-term cost savings by minimizing the need for frequent replacement and extensive corrective maintenance.
B. Pillar Two: Precision Metrology ($\text{Ra}$ and $\text{Rz}$)
The surface finish of the stainless steel hospital sink is a critical, yet frequently incomplete, design specification.
1. The Limitation of Average Roughness ($\text{Ra}$)
Relying solely on the Average Roughness ($\text{Ra}$) value is a technical pitfall. $\text{Ra}$ is a statistical averaging parameter that assesses overall smoothness. While useful (3-A Sanitary Standards mandate a maximum $\text{Ra}$ of 0.8 $\mu\text{m}$ for certain surfaces 7), it provides insufficient detail because it masks isolated surface defects—specifically outliers, scratches, and microscopic pits. These isolated defects, caused by inconsistent fabrication techniques, are the prime locations for bacterial adhesion, serving as the initial anchoring points for biofilm establishment.
2. The Absolute Necessity of $\text{Rz}$
To guarantee clinical efficacy, technical specifications must incorporate the Maximum Height of Profile ($\text{Rz}$). $\text{Rz}$ is a critical safety metric that measures the distance between the highest peak and the lowest valley on the surface. Specifying both $\text{Ra}$ and $\text{Rz}$ is a non-negotiable requirement for critical hygienic components because $\text{Rz}$ quantifies the depth of the microscopic defects (outliers) that $\text{Ra}$ misses, but which are readily exploited by pathogens.
Research confirms that achieving surfaces with lower roughness values significantly restrains bacterial adhesion. This confirms that precision surface finish metrology is the most cost-effective form of preventative hygiene available in infrastructure design.
C. Pillar Three: Integrated Ergonomics and Containment
A sluice sink’s clinical effectiveness is only as robust as the staff workflow it supports. Advanced hygienic design must incorporate human factors to serve as an error-proofing mechanism.
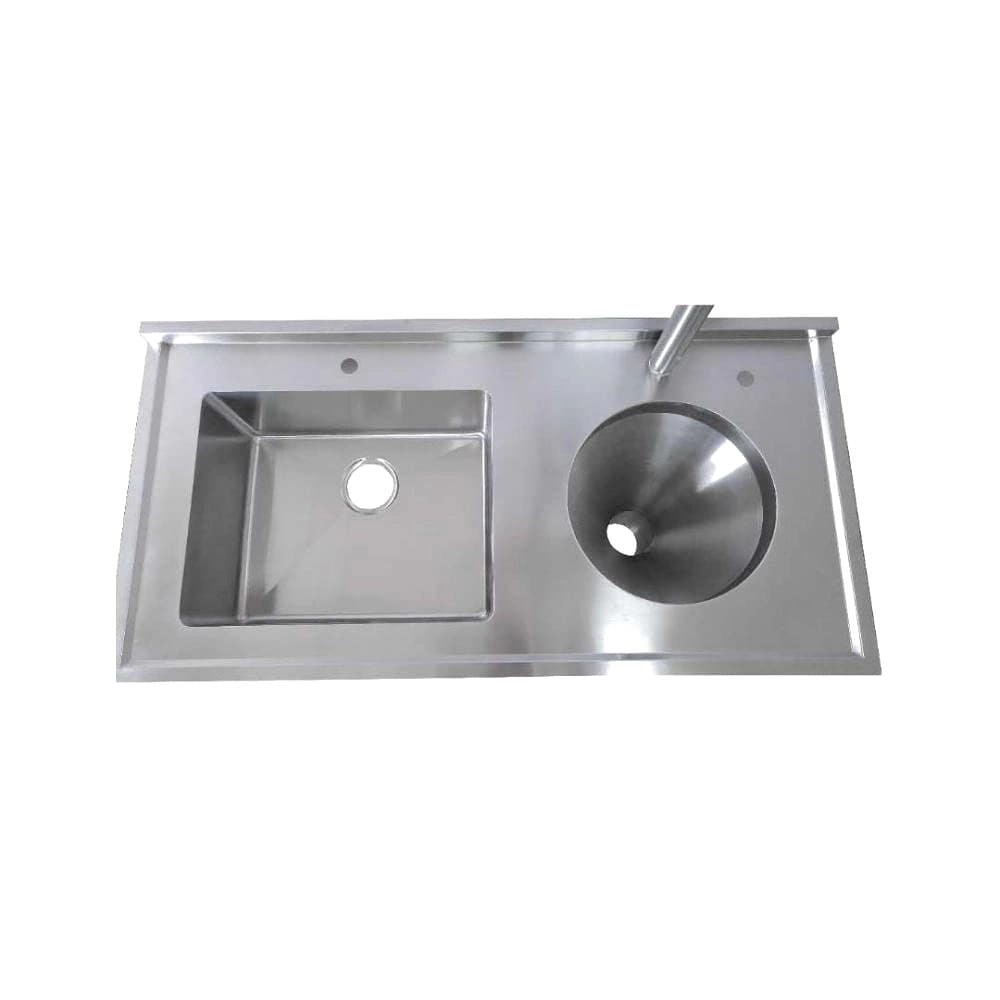
1. Active Waste Containment Features
Hygienic design prioritizes rapid, contained waste disposal to minimize the organic nutrient accumulation necessary for pathogen proliferation 5:
- Conical Flushing Bowl with Seamless Rim: This optimal geometry ensures instantaneous, complete fluid evacuation and biological waste removal.
- Raised Edges: Essential for spillage prevention, actively containing waste within the sluice washing sink basin.
- Off-the-Floor Installation: This feature drastically improves the hospital maintenance team’s ability to conduct comprehensive floor cleaning beneath the unit, eliminating inaccessible microbial reservoirs.
2. Ergonomics as an IPC Strategy
Ergonomic design minimizes the physical strain that leads to manual error and fatigue in high-stress environments.
- Non-Contact Operation: Emphasis on hands-free flush valves and elbow-friendly tap actuation 9 fundamentally reduces the risk of staff-mediated cross-contamination at critical touch points.
- Optimized Workstation: Designing for human factors includes optimizing bench height (e.g., 900 mm) and providing adequate foot clearance for prolonged scrubbing tasks.
This strategic investment in superior ergonomics yields direct, quantifiable returns in reduced infection events and improved operational efficiency, securing patient safety and future financial performance.

III. A Practical Guide: Auditing Clinical Risk in Existing Sinks
For facilities management teams and hospital maintenance staff, assessing the clinical risk of existing sluice sinks requires moving beyond simple compliance documentation.
A. Your Clinical Efficacy Audit Checklist
| Audit Criterion | Minimum Compliance (Baseline) | Clinical Efficacy Standard (Risk Assessment) | Strategic Rationale |
|---|---|---|---|
| Material Grade | Is it Stainless Steel? (Usually SS 304) | Is it SS 316? Are there signs of micro-pitting or corrosion? | SS 316 is mandatory for chemical resilience against cleaning agents. |
| Surface Finish | Does it meet a No. 4 polish? | Is the surface finish specified with both $\text{Ra}$ and $\text{Rz}$ control? | $\text{Rz}$ eliminates critical defects (outliers) that anchor biofilms. |
| Waste Containment | Is the basin size compliant with spatial standards? | Does the design minimize sink basin depth and include a conical flushing bowl? | Mitigates aerosolization risk and ensures complete fluid evacuation. |
| Operational Interface | Are the taps functional? | Is the operation hands-free (non-contact flush, elbow-actuated taps)? | Reduces the highest risk factor: staff-mediated cross-contamination. |
| Environmental Access | Is the surrounding area clear for cleaning? | Is the sink off-the-floor installation to ensure total floor disinfection? | Eliminates floor-level microbial reservoirs and improves operational efficiency. |
B. Common Red Flags Signaling Microbiological Failure
Facilities procurement and maintenance staff must be trained to identify subtle signs of material and microbiological failure that signal a compromised system:
- Pitting or Discoloration: Any sign of reddish-brown corrosion, especially around weld lines or near drains, indicates that SS 304 has failed and pathogen persistence is highly likely.
- Visible Cracks or Compromised Seams: Poorly executed welding techniques create anaerobic spaces where moisture and waste collect, guaranteeing biofilm establishment.
- Chronic Slow Drainage: Indicates consistent build-up of organic matter and biofilm matrix within the plumbing, a key pathogen growth indicator.
- Surface Roughness: Even small areas of roughness or material degradation create ideal sites for bacterial colonization, defeating the purpose of expensive chemical treatments.
When these red flags are identified, administrators must weigh the strategic options. While strengthening staff training and reinforcing infection control protocols is necessary, it cannot compensate for fundamentally compromised hygienic equipment. For sinks showing signs of chronic corrosion or made from substandard materials, replacement with a high-efficacy sluice sink is the most reliable pathway to secure patient safety and achieve TCO objectives.
IV. Investing in Total Cost of Ownership (TCO)
A. The Financial Leverage of Cost Avoidance
The most compelling argument for investing in a high-efficacy sluice sink is not quality alone, but verifiable cost avoidance. The investment must be positioned as an effective insurance policy against the high financial volatility of HAIs.
The Return on Investment (ROI) for superior sluice sink infrastructure is almost immediate. A single high-mortality, environmentally linked infection, such as a Central Line-Associated Bloodstream Infection (CLABSI), carried a per-case cost of over $45,000. By preventing just one or two such events, the increased initial investment is rapidly recovered, transitioning the manager from a cost center to a strategic financial risk manager.
| Financial Indicator | Minimum Compliance Standard: Cost Burden | Clinical Efficacy Standard: ROI & Cost Avoidance |
|---|---|---|
| HAI Risk Liability | High: Annual US cost of HAIs ($28.4B – $45B). A single CLABSI case costs over $45,000. | Low: ROI is often recovered upon preventing just one or two high-cost infections, achieving massive cost avoidance. |
| Material Lifespan | Low: Premature material degradation (SS 304) requires early replacement CAPEX and chronic repair. | High: Extended operational lifespan due to chemical resilience (SS 316) and sustained surface integrity. |
| Operational & Labor Cost | High: Poor ergonomics, manual error, and high spillage increase staff time and process revision requirements. | Low: Optimized staff workflow through error-proofing design and hands-free operation reduces labor and cleaning costs. |
The evidence is clear: the cost savings derived from rigorous infection prevention, improved operational efficiency, and compliance drastically outweigh the initial construction and equipment expenses. This necessitates a strategic reappraisal of capital procurement budgets, shifting the focus from low initial cost to long-term operational solvency.
V. Immediate Action: From Auditing to Specification Upgrade
Decision-making should not be delayed. We strongly recommend that facility managers and procurement officers immediately take the following steps to elevate their infrastructure standards:
- Launch Audit: Use the Clinical Efficacy Audit Checklist (Section IV) to conduct a rapid, risk-based assessment of sluice sinks in critical hospital areas.
- Revise Specifications: Collaborate with infection control and clinical departments to write core performance standards—including SS 316, Rz parameters, and non-contact operation—into future equipment procurement specifications.
- Quantify Risk: Calculate the potential HAI-related financial risk posed by existing defective equipment to build a robust business case for strategic upgrade investments.
- Consult Experts: Introduce technical experts, specifically those with dual expertise in infection control and materials engineering, early into the design phase of major projects.
VI. Defining the Next Culture of Patient Safety
The ultimate takeaway is clear: In the battle against HAIs, minimum regulatory compliance offers a false sense of security. True risk mitigation requires a strategic shift from optimizing initial CAPEX (Capital Expenditure) to managing Total Cost of Ownership (TCO). The solution lies in engineering clinical sluice sinks built on three non-negotiable standards: Material Excellence, Surface Precision, and Hygienic Design.
This is more than an equipment upgrade; it is a strategic investment that converts infection control from a reactive response into a proactive defense secured by the infrastructure itself. Ultimately, this approach champions patient safety and safeguards the organization’s long-term operational solvency and financial health.